
A qualitative study using in-depth semi-structured interviews with implementation stakeholders was conducted to assess experiences and context at select sites (Aim 2). Variation in, and factors associated with severe maternal morbidity were quantitatively evaluated across hospitals using the Michigan Inpatient Database (Aim 1). An explanatory sequential mixed methods design informed by implementation science using the Tailored Implementation for Chronic Disease framework served as the basis for analysis of bundle implementation in Michigan hospitals between 20. The work presented in this dissertation assesses patient outcomes and factors that influenced the bundle implementation process across Michigan hospitals. Since 2016, over 80 hospitals in Michigan participated in implementation of the Alliance for Innovation on Maternal Health’s obstetric hemorrhage patient safety bundle. However, little is known about the real-world impact of bundles, including the optimal context, resources, and processes associated with implementation performance. Bundles present a structured way of improving the processes of care and include a set of evidence-based action steps that, when performed correctly and reliably, may contribute to improved patient outcomes. Nationally endorsed collections of evidence-based practices called patient safety bundles were developed to address this complex issue. Contributing to this problem are a combination of factors including disparities in patient socio-economic characteristics, changing population demographics, variation in medical practice, a fragmented healthcare system, and lack of quality reproductive health data. The United States has the highest rate of maternal mortality despite outspending all other resource-rich countries in per-capita reproductive health care. Study findings prove that it is time to design new care models for PLWH, affected by one or more chronic conditions, both to prevent their onset and to manage their comorbidities. The use of administrative data, combined with a Population Health Management approach represents a powerful tool for evaluating system capacity to manage HIV comorbidities. Adherence to diabetes standards of care tested within the same population was low, with the exception of those tests commonly administered for standard HIV follow-up care. Thirty-one cases of HIV patients diagnosed with diabetes were identified, a prevalence ratio of 4.2% compared to the 8% in the overall population. HIV-related treatments, comorbidities and health service utilization were measured, as was adherence to clinical guidelines-recommended standards of care for diabetes.Ī population of 738 cases were identified in two Local Health Authorities in Italy, representing a prevalence of 0.14% of the general population, in line with the expected prevalence. This retrospective observational study was performed on administrative health data retrieved from 2014 to 2016, with a validated algorithm to identify patients with HIV using: (i) hospital discharge records (ICD9-CM codes) (ii) drug dispensing records (with ATC codes) and (iii) disease-specific exemptions from co-payments for healthcare services. Diabetes represents a paradigmatic case for tackling chronic care management in this target group. This study aimed to measure adherence to diabetes mellitus standards of care provided for people living with HIV (PLWH). The success of antiretroviral therapies has made human immunodeficiency virus (HIV) a chronic disease, changing the care scenario dramatically. 1 Based on these premises, this study aimed to identify PLWH and investigate their healthcare consumption patterns using administrative databases to better understand how care is delivered in different areas of Italy. PHM worldwide has been gaining momentum due to the pandemic of chronic conditions, 9 which, thanks to advances in treatment, now also includes HIV.

7 In short, the segmentation and profiling of the population based on the disease burden and risk profile represent the baseline tools that PHM can exploit in pursuing health service delivery goals regarding improving care at the individual and population levels while controlling costs, as outlined in the Berwick et al.
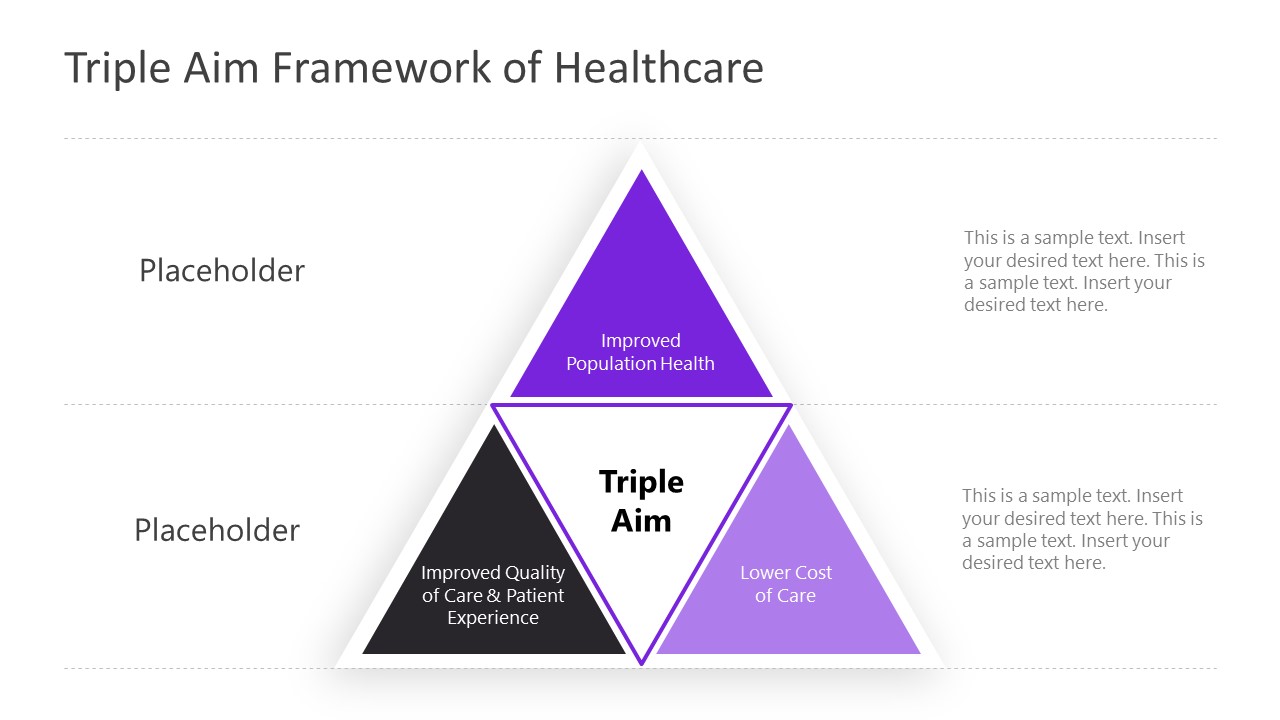
A useful and innovative approach for globally addressing the present and future needs of PLWH is embodied in Population Health Management (PHM), which aims at combining population health needs assessment with effective models of care, in serving those needs, allocating the necessary resources based on risk profiles.


 0 kommentar(er)
0 kommentar(er)
